Interdisciplinary team wins grant to develop drug for brain cancer
March 18, 2022
John H. Rossmeisl, Jr., Dr. and Mrs. Dorsey Taylor Mahin Professor of Neurology and Neurosurgery, Interim Director, Animal Cancer Care and Research Center John H. Rossmeisl Jr.

The National Institutes of Health is awarding a $3.8 million grant to John Rossmeisl, the Dr. and Mrs. Dorsey Taylor Mahin Professor of Neurology and Neurosurgery at the Virginia-Maryland College of Veterinary Medicine, and Waldemar Debinski, cancer biology professor at the Wake Forest School of Medicine. The team will treat human brain cancer with a drug they have previously used to treat canines.
Over the course of five years, the grant will allow Rossmeisl and Debinski to hone a new method to treat glioblastoma, an aggressive and deadly form of brain cancer. The first two years will continue their research on treating canine glioma, and the last three years will treat patients in a clinical trial at Wake Forest Baptist Comprehensive Cancer Center.
The research will characterize in-depth the antitumor activity, safety, and pharmacokinetics of the drug Rossmeisl and Debinski have used in their canine cancer research.
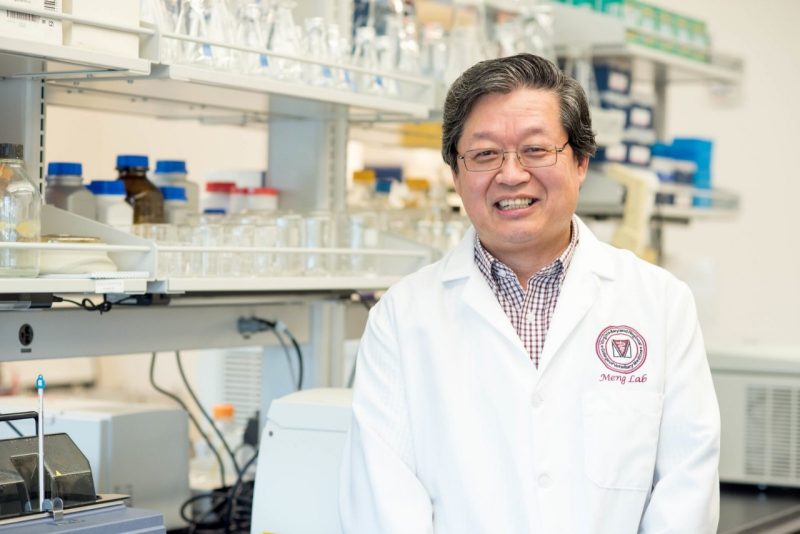
Rossmeisl is the interim director of the Animal Cancer Care and Research Center, a state-of-the-art clinical and research facility in Roanoke and one of the college’s three hospitals. Additionally, he serves as the associate department head of the Department of Small Animal Clinical Sciences and heads the Veterinary and Comparative Neuro-oncology Laboratory. He has collaborated with Debinski, director of the Brain Tumor Center of Excellence at Wake Forest School of Medicine’s Comprehensive Cancer Center, since the early 2000s.
An earlier version of the drug previously went through human clinical trials, but it unfortunately failed. It cannot be given orally or injected, which presents a challenge.
“One of the major reasons why that clinical drug trial failed was not because the drug isn’t effective against the tumor — it just wasn’t delivered effectively to the target,” explained Rossmeisl.
The team has refined a technique called convection-enhanced delivery (CED) to place catheters into the tumor tissue to administer the drug directly. The approach significantly improved the ability of the CED technique to efficiently and effectively deliver drugs to glioblastoma compared to previous trials, which has been fundamental to evaluating the safety and preliminary efficacy of the drug in dogs.
The version of the drug used in the previous human trials targeted one receptor in the tumor. The version in the upcoming trials targets four. The drug not only kills the cancer cells, but when the cells die, the immune system initiates an immune response, killing the tumor more effectively. Part of the grant will be used to better characterize what that immune response is in addition to further refining the delivery method through mapping and modeling.
The team recently finished a canine clinical trial that examined the toxicity of the drug. The team gave six times higher a dose than that which has been given to humans with no toxicity, and results of early trials showed that half of the dogs experienced tumor shrinkage, a remarkable achievement.
This research aligns the college’s One Health approach to veterinary medicine, which recognizes the dynamic interdependence of human, animal, and environmental health and promotes interdisciplinary collaboration.
“Personally, this is the ultimate embodiment of what I want to do. I put something in dogs that not only helps dogs, but it might help someone’s father, mother, sister, brother, daughter, or son. If you statistically look at cancer clinical trials, the odds are stacked against us. But to me, that’s far less important than the fact that at least we’re going to try,” said Rossmeisl.